This guide will focus on the effectiveness of AposTherapy, a novel conservative treatment option available to return patients to function after meniscal tears in the knee.
Contents
- AposTherapy guide
- The meniscus
- Meniscal tear - diagnosis and symptoms
- How does AposTherapy work?
- Treatment options post-meniscal tear
- AposTherapy post-meniscal tear
- Post-treatment follow-up
- Conclusion
AposTherapy guide
AposTherapy is a non-surgical, drug-free treatment for knee pain administered by physiotherapists with specialist training. AposTherapy is used to treat a variety of knee and lower limb conditions; however this article will focus specifically on the success AposTherapy has seen as a treatment for meniscal tears of the knee.
The meniscus
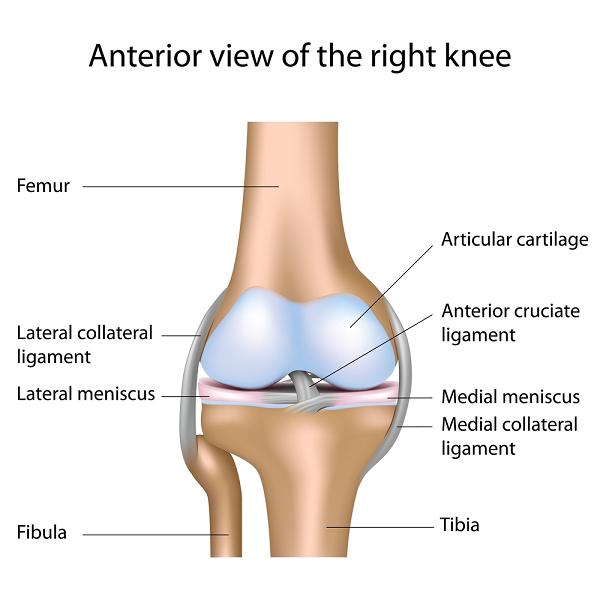
The meniscus is a wedge-shaped, cartilaginous structure found between the articular surfaces in the knee joint. It plays a major role in shock absorption in the knee and biomechanics of the joint movement; the meniscus also holds many receptors that relay information to the brain about the location of the joint and the loads being passed through the joint. This information travels to the brain via the nervous system. The brain then decides on the appropriate muscular reaction in order to control the knee, stabilise it and avoid injury. This control is vital to avoid injury and damage to structures in and around the knee joint.
Meniscal tear - diagnosis and symptoms
Meniscal tears are the leading cause of knee injury (1) and can be categorised into two types:
- Degenerative tears
- Traumatic tears, often seen in patients under the age of 35 years (2)
Degenerative tears have been seen in 60% of the patients diagnosed with osteoarthritis (OA) over the age of 65 (2), and are usually caused by low-level activity. Nonetheless, studies have shown that there is very little correlation between the presence of a tear in the meniscus and the patient’s pain and difficulty with daily functions. Over the age of 65, many people have meniscus tears but experience very little or no pain (3).
In some cases, in the acute phase after a meniscal tear has occurred, there will be severe pain on weight-bearing, sensations of instability and muscle bracing of the injured limb and trunk (1). This results in an altered walking pattern after a meniscal tear. It has been shown in research that up to three months after the injury, an average difference of 1.5% in the proportion of time spent on each leg is measured by computerised gait analysis (4). This difference may put the other leg at risk as it bears more weight in every activity that person performs. A decrease in the step length of the involved leg is also seen, this reduction is caused by the bracing of the hamstring muscles at the back of the leg that keep the knee bent (4). These effects on the walking pattern result in a decline in quality of life and physical function (1).
A degenerative tear can be diagnosed according to the mechanism of injury, special tests performed by a healthcare professional, and in many cases MRI scans are performed to determine the location and extent of the tear.
How does AposTherapy work?

AposTherapy involves the use of an individually calibrated foot-worn biomechanical device. The device must be calibrated by an AposTherapist; a specially-trained physiotherapist. This process can only be completed following a thorough subjective assessment, an objective computerised gait analysis and a physical assessment of the injured and surrounding joints. During the calibration of the biomechanical device using Pertupods on the base of the shoes, two principles are integrated into the system to achieve the correct muscular control.
The first principle involves adjusting the placement of loads. Following a meniscal tear the therapist aims to move the loads away from the damaged area of the meniscus to reduce the pain.
The second principle introduces a mild instability that stimulates a co-ordinated response from the surrounding muscles, thus resulting in improved joint stability throughout the walking cycle.
Patients can commence the treatment at differing intervals after the meniscal tear; the Apos System can be individually adjusted according to the duration of time that has passed since the injury was sustained. By adjusting the calibration of the Apos System, the biomechanical loads passing through the joints will be altered with the aim of reducing pain and preventing a gross asymmetry in walking patterns. It has been shown in research that the use of AposTherapy following a meniscal tear successfully improves the gait pattern on the injured limb as well as improving the symmetry of gait (4). We would expect these benefits to lead to a reduction in compensations at other joints and to assist the recovery process.
The AposTherapist will provide the patient with a personalised therapy programme outlining how the individually-calibrated system should be used in the home and/or the office environment. This will involve a short duration of use each day tailored to the patient’s condition, goals and daily routine.
Each patient will set goals when they commence the treatment; these goals may relate to hobbies, social activities or work. To ensure that the patient successfully achieves these goals it is critical that the treatment progress is monitored and adjusted as the patient progresses through their programme. This monitor and re-assessment is completed through a series of follow-up appointments; each patient attends approximately five follow-up consultations during a year’s course of treatment.
Treatment options post-meniscal tear
There are a variety of treatments available for meniscal tears, many of these provide benefits through pain relief, reduction in inflammation and in the case of arthroscopies (keyhole surgery), the removal of the damaged part of the meniscus. An arthroscopy has been seen as a popular treatment option however according to the National Institute of Health and Clinical Excellence (NICE) Guidelines an arthroscopy is only recommended for a certain type of meniscal tear that causes mechanical true-locking of the knee joint (5). This type of meniscal tear is much more prevalent in younger, highly active individuals. After an arthroscopy, the meniscus itself cannot heal like other tissues in the body such as bone and skin. This means that even after removing the damaged part, a certain degree of pain may remain. These treatments do not address impaired nerve and muscular control patterns implemented around the joint after a meniscal tear.
Traditional physiotherapy is a common treatment used to improve the impaired control patterns of muscles. Physiotherapy utilises the principles of motor learning to retrain the neuromuscular system. Effective and efficient motor learning requires functional, task-specific, subconscious and high-repetition movement. The main barrier encountered during physiotherapy treatment following a meniscal tear is the ability to perform enough repetitions in a truly functional, subconscious manner thus limiting the ability to teach the neuromuscular system to provide the joint control patterns required to cope with the injury.
AposTherapy post-meniscal tear
AposTherapy aims to address the impaired control patterns that the muscles use following meniscal tears. It is non-invasive and drug-free meaning that it is very safe.
AposTherapy embodies the principles required to efficiently retrain movement patterns; achieving thousands of repetitions of subconscious, functional movements while implementing improved muscular control patterns becomes convenient through the use of AposTherapy.
Recently published research has shown that AposTherapy significantly reduces the pain experienced due to knee osteoarthritis (OA) and improves function. In addition to subjective improvements in pain and function, AposTherapy is successful in restoring symmetry to the walking pattern after a meniscal tear (4). Elbaz and colleagues performed a retrospective analysis of 34 patients with knee osteoarthritis (OA) and a degenerative meniscal tear to determine the effect of 12 months of AposTherapy. The study found an improvement in walking velocity, step-length and single-limb support (the proportion of time spent on each leg during the gait cycle) compared to the normal values, as well as improved symmetry in the limbs throughout the walking cycle (4). In addition to the computerised gait analysis, Elbaz also monitored pain, stiffness, physical function, physical health and mental health through the use of questionnaires such as the Western Ontario and McMaster Universities Arthritis Index (WOMAC). Analysis of survey results concluded that AposTherapy is a suitable treatment for meniscal tear in patients with knee OA (4). The study questioned participants at the start of treatment, at three months and twelve months and concluded that the positive effects AposTherapy achieved were also maintained after a year of treatment (4).
A reduction in quality of life is often reported following a meniscal tear, however, by improving the walking pattern and reducing the pain, function improves thus maintaining or improving quality of life. By achieving symmetry in the walking pattern, the patient is also less likely to develop secondary problems due to compensations at other joints. Finally, by improving the neuromuscular joint control, a less joint degeneration would be expected. By slowing down the natural progression of osteoarthritis, an improvement in the patient’s joint health, function and quality of life will be seen in the long-term. When considering what treatment to choose after a meniscal tear, AposTherapy can reduce pain, and increase quality of life and function after a 12 month period as well as avoid the surgery that these patients were expecting to be required.
Post-treatment follow-up
AposTherapy aims to empower the patient by providing a tool that assists in long-term management of osteoarthritis relating to meniscal tears. Following the first year of treatment, patients’ goals are focused towards maintaining functional improvements and preventing joint damage in the future. To achieve these goals, the AposTherapy programme encourages regular continued use but requires a less structured therapy programme. Continued use of AposTherapy to manage a chronic knee condition ensures the improved neuromuscular control patterns are maintained with the aim of preventing further joint deterioration. Often this stage is acquired quite naturally due to the convenient, routine integration of AposTherapy in their day-to-day activities. During this stage, many patients choose to continue follow-up consultations at 3–4 month intervals to make use of the monitoring systems, questionnaires and computerised gait analysis, as well as to gain guidance regarding the optimal use of their biomechanical systems and a review of the system calibration as their condition evolves with time.
Conclusion
Meniscal tears are a common complaint; they can present with a variety of symptoms and often cause a reduction in function and quality of life. Surgical treatment of meniscal tears is a common treatment option, however it is often not necessary and does not address the neuromuscular impairments that exist following a meniscal tear. Recent research strongly supports the use of AposTherapy to reduce pain and increase function post-meniscal tear (4) through functional neuromuscular retraining.
References
1. Rodkey WG. Basic biology of the meniscus and response to injury. Instructional Course Lectures 2000;49:189-93
2. Meniscal Tears. American Academy of Orthopeadic Surgeons February 2009
3. Englund M, Guermazi A, Gale D, Hunter DJ, Aliabadi P, Clancy M, Felson DT. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. New England Journal of Medicine 2008;359(11):1108-15
4. Elbaz A, Beer Y, Rath E, Morag G, Segal G, Debbie EM, Wasser D, Mor A, Debi R. A unique foot-worn device for patients with degenerative meniscal tear. Knee Surgery, Sports Traumatology, Arthroscopy May 2012
5. NICE Clinical Guideline 59: Osteoarthritis








