Mr Philip Stott, Consultant Orthopaedic Surgeon, discusses his approach to hip replacement surgery. 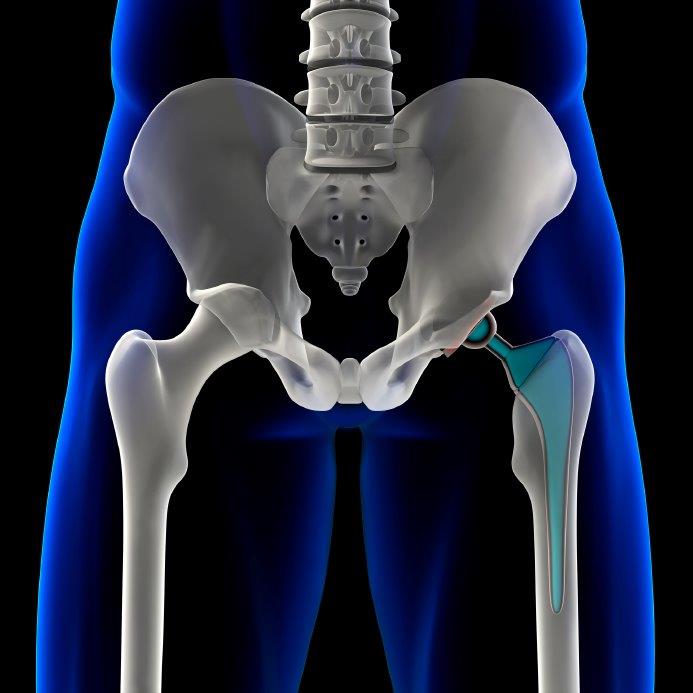 He specialises in primary and revision hip replacement surgery and hip replacement in younger patients.
He specialises in primary and revision hip replacement surgery and hip replacement in younger patients.
Total Health asks ten top hip Consultant Surgeons the following questions:
- Q1: Which type of hip prosthesis do you routinely use and why?
- Q2: How long have you used this choice of hip replacement?
- Q3: Do you use this hip prosthesis exclusively?
- Q4: If you sometimes use alternative hip prostheses please specify which type(s) and why?
- Q5: What hip procedure do you use?
- Q6: If you needed a hip replacement now which prosthesis and procedure would you opt for?
- Q7: What over-riding piece of advice would you give to someone considering having hip replacement?
Q1: Which type of hip prosthesis do you routinely use and why?
Whilst orthopaedic surgeons perform large volumes of hip replacements, no patient should ever be considered 'routine'. Having hip surgery is a major undertaking for any patient. Most patients do not consider themselves ‘routine’.
No patient considers themselves as routine
I therefore talk to every patient to discuss which hip replacements are suitable for them, looking at the latest best available evidence as to the best performing implants. A patient does not want a hip that will only last a few years, or even ten, but one that has been used in real patients and has proven its effectiveness. To identify these best performing hips, one has to look in the Joint Registries of different countries, and also to published studies about prosthesis performance and longevity.
All of the joint registries demonstrate that cemented implants do better in terms of both longevity and lower complication rates than cementless hips. Hip surgery continues to evolve, and new products appear on the market regularly. We have seen time and time again how some of these new hips fail early (often less than 8 years) despite having excellent theories behind them. I prefer the Exeter hip. This has a survival rate for the stem of at least 90% at 33 years (http://eprints.qut.edu.au/18942/3/18942.pdf) The Exeter has a range of sizes that allow me to accurately reproduce a patient’s anatomy. It is also the best performing hip in England and Wales according to our National Joint Registry (page 49, 14th Annual Report) (http://www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/11th_annual_report/NJR%2011th%20Annual%20Report%202014.pdf)
Some patient’s anatomy / lifestyle however does not suit a cemented hip, and then I would offer them a cementless implant. The choice of implant again depends on the patient’s needs. Literature would support the Jri Furlong HAC hip, as this has proven results both in the literature and in the National Joint Registry. (http://www.jri-ltd.co.uk/healthcare-professionals/furlong/results.aspx#)
I use a lot of ceramic bearings in my practice – a ceramic head with a ceramic or a plastic cup. I used to offer resurfacing hip operations, but with concerns over metal ions and the damage that they can do, I no longer perform enough of these surgeries to feel comfortable implanting them. I will however discuss this with patients, and if the patient wants one, I will refer the patient to a surgeon that performs high volumes of resurfacing arthroplasty.
Q2: How long have you used this choice of hip replacement?
I was trained in all of these implants (including resurfacing) as a trainee. I have been using all of them since becoming a consultant.
Q3: Do you use this hip prosthesis exclusively?
I use different prostheses on different patients. Sometimes, I will have 5 patients on my operating list, and each will get a different prosthesis!
Q4: If you sometimes use alternative hip prostheses please specify which type(s) and why?
Sometimes a patient has to have a complex operation where I will need to shorten their leg. I use a Depuy S-ROM for this. Occasionally a patient has very abnormal anatomy, and I will have a custom implant made for them. When I perform a hip replacement in a teenager, I have different expectations for these hips, as I will expect the hip replacement to wear out. I therefore want a hip that will be relatively easy to remove, without doing the patient too much damage. I will then use a cementless hip such as an Accolade.
Q5: What hip procedure do you use?
I use a minimally invasive posterior approach in a team setting where we follow the principles of enhanced recovery. This allows a patient to get back to what they want to be doing more quickly. We minimize the surgical and anaesthetic trauma to a patient, and give them evidence based physiotherapy treatments, whilst supporting their recovery.
Q6: If you needed a hip replacement now which prosthesis and procedure would you opt for?
If my anatomy allowed it, I would have a cemented Exeter with a ceramic bearing. I have had patients climb mountains, play football and tennis to high levels and ski with this option.
Q7: What over-riding piece of advice would you give to someone considering having hip replacement?
Most patients find that having a hip replacement is a life changing operation. However, the patient needs to be aware of all of the risks and benefits of an operation. Complications are rare, but do occur. The patient should not leave it so late that all of their muscles have disappeared and the joint has become so stiff that a new hip will not regain a good range of motion. It is important to be as fit as possible for your operation The quality of the surgeon is at least as important as the implant used. We have reliable data on implants. To help you identify a quality hip specialist in your area, ask friends / relatives / patients who have had hip replacements and your General Practitioner.
Your surgeon should be performing over a hundred hip replacements a year. Individual Surgeon results on the National Joint Registry have a natural inaccuracy. The more complex hip cases have a much higher complication rate than a standard hip replacement. These complex cases are not filtered out of the published results, and you cannot tell if those reported complications are on standard cases or complex ones.
See also answers from the following hip replacement experts:
- Mr Howard Ware
- Mr Ed Davies
- Mr Mark Rickman
- Mr Jeremy Latham
- Mr Paul Jairaj
- Mr Stephen Jones
- Mr Warwick Radford:
- Miss Samantha Tross
- Mr Charles Willis-Owen
- Mr Winston Kim











