This article presents an overview of an innovative treatment for overactive bladder, sacral nerve stimulation. This new treatment can cure incontinence and pelvic pain syndrome without the need for drugs or surgery.
Contents
- What is sacral nerve stimulation?
- What conditions can be treated by sacral neuromodulation?
- What does the treatment involve?
- How does the treatment work?
- How does it feel?
- What is the evidence for this treatment?
- How effective is it?
- Frequently asked questions
- Further reading
What is sacral nerve stimulation?
Sacral neuromodulation is a new treatment, which was approved for use in the United Kingdom in 2004, but has only recently been authorised by local authorities and private insurers. Also known as sacral nerve stimulation (SNS) it uses electrical currents to reset the faulty nerves causing bladder dysfunction.
“Sacral nerve stimulation is a very important breakthrough in the treatment of the overactive bladder and pain syndromes. This new technique provides an effective solution for women when conservative treatment has not worked. It avoids the necessity of repeated treatment with Botox, and the risk of catheters with Botox and major surgery.”
Jeremy Ockrim, Consultant Urologist, University College Hospital and Harley Street, London
What conditions can be treated by sacral neuromodulation?

Overactive bladder and voiding dysfunction
Overactive bladder is a common complaint in women and can affect men too. Bladder spasms cause frequency-urgency and urge incontinence. Over 30 per cent of women (and 10% of men) will experience problems with continence, typically after childbirth and menopause, although younger women can also be affected.
Voiding dysfunction in young women (sometimes called Fowler’s syndrome), is a rare condition resulting in an inability to relax the sphincter causing retention of urine and catheter dependence.
Pelvic pain syndrome and interstitial cystitis
The causes of pelvic pain are not well understood and in most cases a specific cause is not identified. Interstitial cystitis is an inflammatory condition of the bladder comparable to arthritis of the joints or colitis of the bowel. The condition leads to pain as the bladder fills, resulting in frequency urgency and chronic pain.
What does the treatment involve?
The first step is to have a test procedure to see whether SNS will be effective for you.
The nerves are located in the lower back, adjacent to the sacrum. Under a short general anaesthetic (or occasionally local anaesthetic), the surgeon uses a small needle to place a thin wire in contact with your sacral nerves. The other end of the wire is tunnelled under the skin or taped to the back and connected to a temporary stimulator control unit, which is worn on your belt. The temporary stimulator is worn for four weeks to assess your response. The approach works well for approximately 70 per cent of patients.
If you find the treatment effective, you will be asked to come into hospital again to have a permanent implant. This is a much smaller device – the size of a £2 coin – which is implanted under the skin and fat of the lower back so it cannot be felt. You will not have to have anything attached to your back or any external device. A control unit, the size of a mobile phone, is used to change and control the frequency of electrical signals and you can keep this at home. The infection rate for this procedure is less than 1%.
The procedure is carried out under general anaesthetic, and most patients return home on the same day.
How does the treatment work?
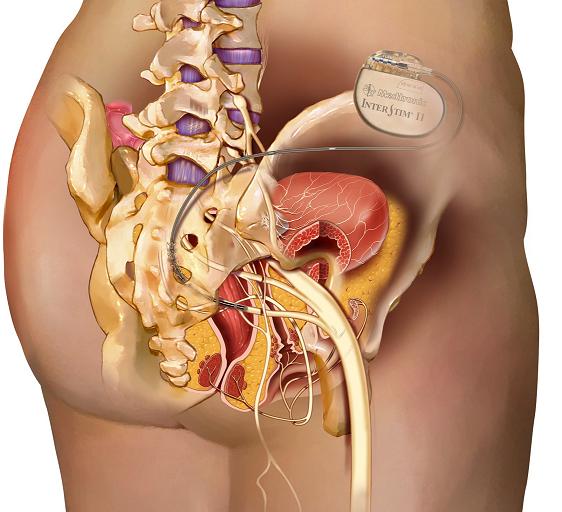
This treatment is sometimes referred to as the ‘pacemaker for the bladder’. A traditional cardiac pacemaker is a device implanted inside the body which sends electrical currents to the heart, correcting faulty heart rhythms.
In an ‘overactive bladder’ the sacral nerves send unwanted messages to the bladder, causing it to contract suddenly (urgency) and empty without due warning (urge incontinence). In voiding dysfunction the reverse happens preventing the sphincter from relaxing. Sacral nerve stimulation works by interrupting this ‘faulty circuit’ and restoring normal communication between the nerves, brain, and bladder. In pelvic and bladder pain the same nerves conduct the pain signals to the brain. Electrical stimulation at the nerve roots dampens these signals and reduces pain in 40–70% of sufferers.
Unlike Botox, there is no need for repeat treatment, and there is little risk of requiring catheters to empty your bladder. The battery in the permanent implant is effective for up to seven years.
How does it feel?

The implant is very small and placed underneath the fat of the lower back / upper buttock area. The surgeon makes a small incision of about 3cm to insert the device during surgery, so recovery is quick and straightforward. The device is cushioned by the body’s fat and so you will not be aware that you have any implant in that area although some patients say they are sometimes aware of the device when they lie in certain positions. In 5–10% of patients the device can cause discomfort and its position needs to be adjusted. The electrical stimulation is kept below detectable levels and the patient is not aware of the stimulation unless the pulses are turned up. There is usually an initial period for the first few weeks after the implant is inserted when you are getting used to the device and finding the right level for you.
Sacral nerve stimulation is also used to treat bowel frequency and urgency – a problem that is often associated with overactive bladder. SNS is also reported to help sexual dysfunction and improve sexual sensitivity for women.
What is the evidence for this treatment?
Sacral nerve stimulation was first described in 1998 and now has ten years of accumulated evidence establishing its effectiveness and safety. Sacral nerve stimulation was approved by NICE (National Institute for Health and Clinical Excellence) in 2004 and is widely used in Spain, Holland and Germany. However, the technique has not been widely available in the NHS due to cost and limited expertise available in the UK.
To read a patient’s account of their experience of sacral nerve stimulation, click here.
“We have been amazed at our patients’ responses to the new sacral nerve stimulation technique. The implant has revolutionised their lives and allowed them to return to social activities, where they had previously lost confidence. We offer continued after care to adjust the device settings according to our patients’ individual needs.”
Julie Jenks, Specialist Nurse Practitioner, University College Hospital, London
How effective is it?

I work alongside Nurse Specialist Julie Jenks and we have the largest experience of sacral nerve stimulation for bladder dysfunction in the UK. I am the lead specialist for SNS and bladder dysfunction at University College Hospital, London. Together we have treated over 140 patients in the last 12 months and have many more waiting; with the majority finding their urgency and incontinence has significantly improved or ceased, and over 70% proceeding to the permanent implant after a test stimulation.
FAQs
What happens after the implant has been fitted?
The sacral nerve stimulator runs continuously for up to seven years and will be invisible to everybody. Awareness of the neurostimulator will gradually diminish, and you may not even feel its presence. Sometimes, several visits are necessary to fine tune the settings during the first three months. Otherwise, you may only need a yearly check-up.
Is aeroplane travel safe?
Airport screening systems can cause the neurostimulator to turn OFF or ON. It does not change your stimulation parameters. Use your patient programmer to switch your neurostimulator to what it was before. To avoid possible problems with airport screening systems, you may want to show your InterStim identification card and ask those in charge to let you bypass the screening device.
Will the InterStim system limit my activities?
There are specific restrictions while carrying out your activities, but you should avoid activities that involve sudden, excessive, or repetitive bending, twisting, bouncing, or stretching especially soon after the surgery. These movements could damage or move your implanted lead or affect the implanted neurostimulator. Usually, movements do not affect the sensation of the stimulation.
Further reading
1. Herbison GP, Arnold EP. Sacral neuromodulation with implanted devices for urinary storage and voiding dysfunction in adults. Cochrane Database Syst Rev. 2009;15(2):CD004202
2. Van Kerrebroeck et al. Results of Sacral Neuromodulation Therapy for Urinary Voiding Dysfunction: Outcomes of a Prospective, Worldwide Clinical Study. The Journal of Urology. 2007;178:2029-2034
3. Chaabane W et al. Sacral neuromodulation for treating neurogenic bladder dysfunction: clinical and urodynamic study. Neurourology & Urodynamics. 2011;30(4):547-550
4. Gajewski JP, Al-Zahrani AA. The long-term efficacy of sacral neuromodulation in the management of intractable cases of bladder pain syndrome: 14 years of experience in one centre. British Journal of Urology International. 2011;107(8):1258-1264
5. Powell CR, Kreder KJ. Long-term outcomes of urgency-frequency syndrome due to painful bladder syndrome treated with sacral neuromodulation and analysis of failures. The Journal of Urology 2010;183(1):173-176
For further information on the author of this article, Consultant Urological Surgeon, Mr Jeremy Ockrim, please click here.
The time of a woman’s life when her ovaries stop releasing an egg (ovum) on a monthly cycle, and her periods cease
Full medical glossary
