What is Atrial Flutter and How is Atrial Flutter Diagnosed?
The normal beating of the heart is controlled by electrical impulses. Atrial flutter is an abnormal electrical short circuit that results in a rapid or irregular heartbeat. It can occur in either the left or right atrium of the heart, which are the top 2 chambers in the heart. The atria pump blood to the larger ventricles below - to use a motoring analogy, they are bit a like fuel injectors or carburetors.

Contents
- Typical Atrial Flutter
- Clockwise Atrial Flutter
- Atrial Flutter and the Risk of Stroke
- CHA2DS2VAScscore
- How can Atrial Flutter be Identified and Diagnosed?
- Treatment for Atrial; Flutter
- Catheter Ablation
- Atypical Flutter
The most common type of atrial flutter occurs in the right atrium and is known as typical atrial flutter. It is common from around the age of 40 onwards. This is the same heart rhythm disorder that Tony Blair suffered from in 2004, and he went on to have a curative procedure called ablation.
Clockwise Right Atrial Flutter
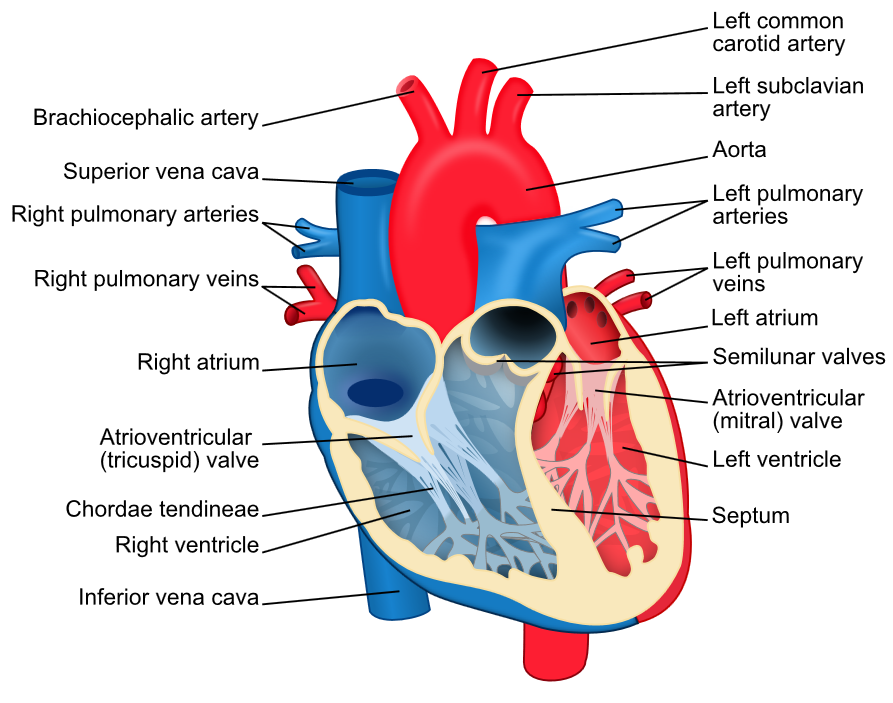
In atrial flutter electricity rotates rapidly and regularly around the tricuspid valve, the valve between the right atrium and right ventricle. It can rotate in an anti-clockwise direction (known as typical flutter), or a clockwise direction (known as clockwise right atrial flutter). The direction of electricity can be identified on a standard ECG.
This means that the atria beat about 300 times per minute, which is about 4 to 5 times faster than normal. Fortunately, most of the time not all of these signals conduct to the ventricles below, but the heart rate still increases to 150 per minute in healthy hearts. This can cause palpitations, breathlessness, dizziness or even collapse.
Atrial flutter and the risk of stroke
When the atria beat 300 times per minute, blood can stagnate within them and this can lead to clot formation in the heart, particularly in an area called the left atrial appendage. This is a tube-like chamber (a bit like the appendix in the bowel) attached to the left atrium. When clots form here they can dislodge and travel through the heart and circulate to the brain, causing a stroke.
To identify patients who are at risk of stroke when they have atrial flutter, we use a scoring system called the CHA2DS2-VASc scoring system.
The CHA2DS2VAScscore is an acronym. It stands for:
C = Congestive cardiac failure (or heart failure or impaired
ventricular function)
H = Hypertension (or high blood pressure)
A2 = Age over 75
D = Diabetes
S2 = Stroke or TIA (transient ischaemic attack, or ‘mini-stroke’)
V = Vascular disease (heart attack or other arterial disease)
A = Age below 65
Sc = Sex category (female = 1 point)
If you have or have ever had one of these conditions you score one point for each, except Age over75 or Stroke/TIA which count as 2 points, hence the CHA2DS2VASCscore.
If you have a CHA2DS2VASC score of 1 or more it is recommended that you take warfarin (or one of the newer types of anticoagulant medications) for life to reduce your risk of stroke, unless the atrial flutter is cured with a procedure called ablation (see below). So, if you are 65 or older and have atrial flutter, it is recommended that you are treated with an anticoagulant and not aspirin, which is now known not to be beneficial.
How can Atrial Flutter be Identified and Diagnosed?
If you develop any of the symptoms described above, a simple ECG (or heart tracing) easily identifies atrial flutter when you are feeling the palpitations. If your symptoms are intermittent, you may need to wear a heart monitor for a longer period of time to try and capture an episode.
Atrial flutter can also be identified in patients with pacemakers or defibrillators when their device is checked.
Very occasionally it is necessary to implant a small heart monitor under the skin to diagnose a patient’s palpitations, if they are very infrequent.
The first line treatment for typical atrial flutter is a procedure called catheter ablation. Ablation is a ‘key-hole’ procedure performed by inserting fine wires through the vein at top of the right leg. The wires record signals from inside the heart and one of them can cauterize heart tissue by heating up at the tip (using something called radiofrequency energy – a bit like microwave energy).
The way typical atrial flutter (or clockwise flutter) is treated is by creating an ‘electrical road-block’ across one part of the abnormal circuit to prevent it from going round and round. Once the line is complete, the flutter stops and a normal rhythm returns. The place where this roadblock is created is between the tricuspid valve and the main vein that connects to the heart from the lower part of the body, called the inferior vena cava. Therefore the ablation is technically called cavo-tricuspid isthmus ablation.
Ablation compared with Medication and / or Elictrical Cardio-version (shock treatment)
Ablation is preferred to medications or electrical cardio-version (shock treatments) because the procedure is highly effective (90% cure with one attempt) and has a very low risk (principally that of injury to a blood vessel at the top of the leg and a 1 in 500 risk of damage to the AV node requiring pacemaker implantation, or making a tiny hole in the heart – requiring drain insertion).
It has been shown in a number of randomised clinical trials that ablation is significantly better than drugs or cardio-version as a first line treatment for typical flutter. It is well known that atrial flutter is very resistant to medications and almost always recurs after cardio-version. The ablation procedure is usually quick (30-60 minutes) and patients can return home the same day. Ablation in this part of the heart can be painful and for this reason it may be performed under general anaesthetic.
There are several other types of ‘atypical’ flutter, which can occur in the left and right atria. These are commonly seen after ablation procedures in the left atrium for another heart rhythm abnormality called atrial fibrillation (or AF for short). They can also occur in patients with congenital heart defects (therefore young patients) or those who have had surgery to the heart.
They too can be successfully treated with ablation, but the ablation procedure tends to be more complex and takes longer to perform. The risk of ablation in the left atrium is slightly higher than that described above.
See Atrial Flutter Ablation FAQs







